Rapid Breakthrough
Using a human-centered, data-driven, collaborative approach we explored how an existing surgical virtual collaboration and training platform could be re-imagined in order to deliver new propositions and benefits in diagnostics pathway.
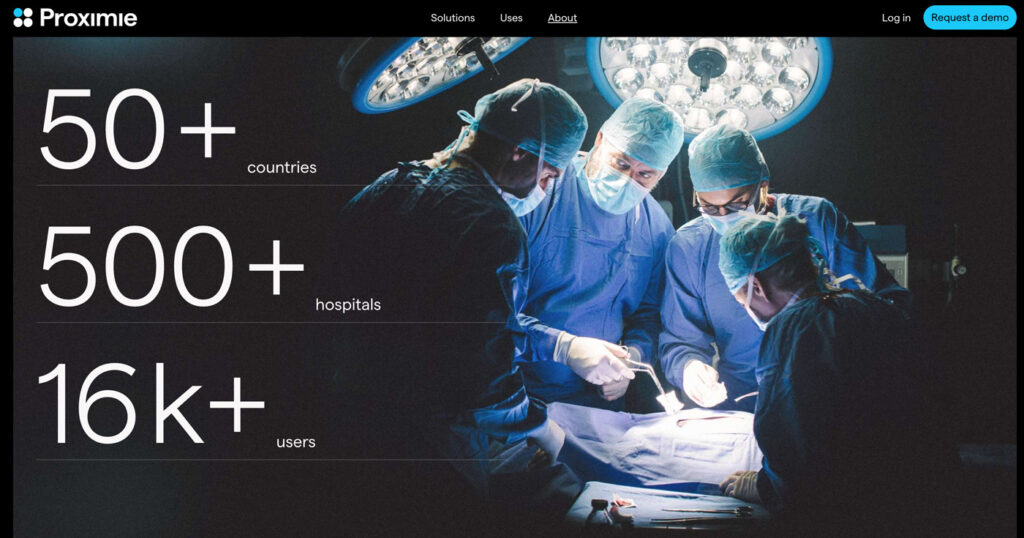
About the client
Our client is a UK-/ USA- based health start-up whose digital healthcare platform brings together telepresencing, content management, and data insights. The platform enables hospitals, surgeons, and device companies to capture operating room data and share information from anywhere, and to generate new insights so they can improve outcomes and productivity.
Problem
A Lancet/ World Health Organisation commission on global surgery estimates that over 5 billion people do not have access to safe surgery. In addition in July 2023, the NHS estimated that over 7 million people were on the waiting list for elective care – i.e. care that is planned in advance and which often involves specialist clinical care or surgery. This figure represents more than one-tenth of the population and is a 30% on figures before the Covid-19 pandemic. It is also a situation that is being played out in both the public and the private sectors and in many nations too, not only the UK.
On top of this, and again a global challenge, is the shortfall in skilled health care staff. In 2019-20 the global shortage in the nursing workforce was estimated as being 27.9 million nurses, a figure that could reach 13 million by 2030.
Shortages of other types of skilled worker also apply in other areas of primary, secondary, social and community care. Concerningly, these figures indicate deep underlying trends and the deep, compacting effect that managing the virus has on the NHS’s delivery of its ’normal services.’


Response
Our client’s purpose is to save lives by creating a ‘borderless operating room’. The business has developed an augmented reality technology allowing surgeons to advise on and direct operations remotely and in real time across the globe. For example, a surgeon working in one location – for instance, a field hospital in a war zone – could access a more experienced surgeon working in a major town or city on demand, in real time to get help on a procedure.
Given this purpose, the issues of a lack of access to safe care delivery generally, and the tsunami of the elective care backlog engulfing many care providers (NHS included), the client team wanted to explore how their technology could be re-imagined in a way that increases care delivery capacity and help reduce waiting lists. They also wanted to better understand how this could be done in a way that reduces the burden on an already over-stretched workforce.
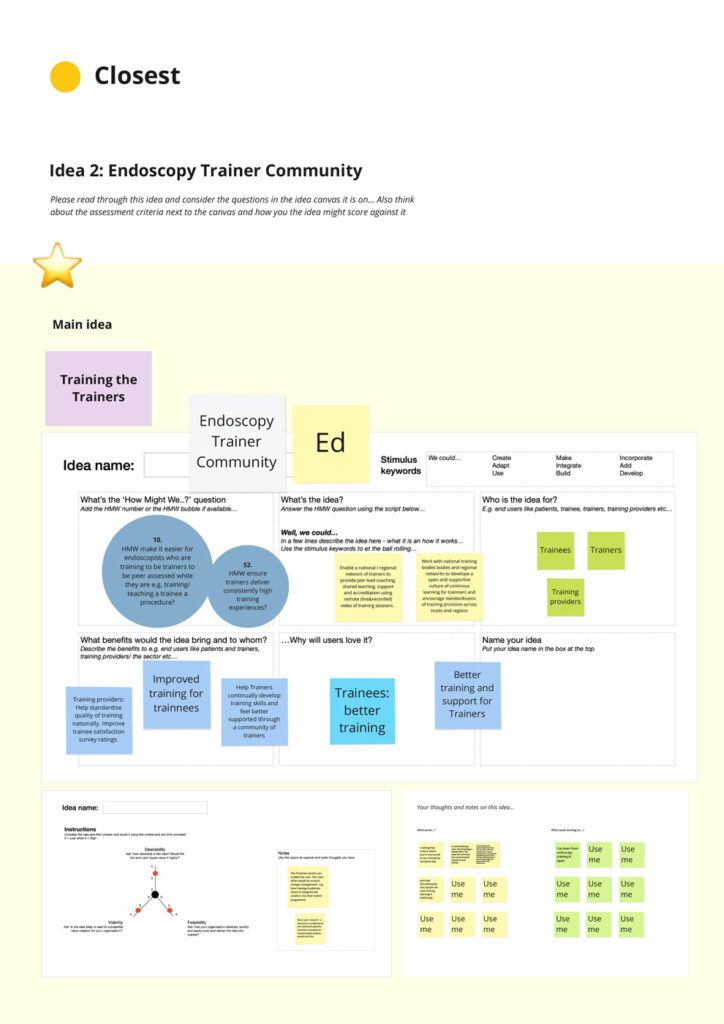
The specific question they wanted to explore was ‘How the existing product be re-cast to train more colonoscopists and so increase diagnostic capacity – i.e. what adjacent services could be offered that increased training capability to enable care to be delivered in a timely, efficient and safe way?’
What we did
To explore the question, we followed our tried and tested human-centred, highly collaborative and mixed disciplinary approach. This included taking the following steps:
- Hypothesis definition to create a focussed design challenge to dig into/ explore
- Recruiting a squad of experts, including patients, technology and healthcare professionals
- Data download and review to identify possible opportunity areas
- Virtual ‘walk a mile’ exercises with patients and relevant medical and technology professionals to blueprint the ‘referral to diagnosis’ experience for patients and colonoscopy trainees
- Identification and technical validation of possible value creation opportunities
- Best Practice research from relevant fields to provide innovation exemplars
- Future portfolio lay-down and roadmapping to identify what could be delivered when
- Analysis to understand how different ideas could work off each other to create extra value
Results
- Clearer understanding of the colonoscopy delivery and training ecosystem
- Deep understanding of opportunities to create value in colonoscopy training pathway
- Accelerated learning about service delivery optimisation and Best Practices
- Deeper connections/ engagement with the colonoscopy community, technology and patient groups
- Prioritised/ de-risked set of new propositions to take into the design, build and release stages
- Clear understanding/ vision of the future landscape, strategic direction and how to get there
- Enhanced investment story – i.e. shortly after this project our client raised an extra $80 million of investment via a Series C investment round (this followed a $38 million Series B round in April 2021 to bring the client’s total funding to $129m)
- Helped with the set-up of technology-enabled endoscopist training pilots in the UK and USA
Collaborators
The project brought together a mix of expert collaborators from different disciplines, organisations and sectors, including patients and patient groups, consultant nurses, data scientists, consultants, service improvement leads and trainers working in endoscopy and gastroenterology in England, Wales and Ghana.
We are particularly grateful to individuals from these organisations and teams:
- Powys Teaching Health Board
- Endoscopy Training Management Group
- St George’s University Hospitals NHS Foundation Trust
- University of Ghana Medical Center
- Service Improvement BICS Team, Bolton Hospital NHS Foundation Trust
- South Tees Hospitals NHS Foundation Trust
- George Eliot Hospital NHS Trust
- University Medical Centers (UMC), Amsterdam
- University Hospitals of Morecambe Bay NHS Foundation Trust

